Heel pain is most often caused by plantar fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst.
Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and determine the underlying source of your heel pain.
What Is Plantar Fasciitis?
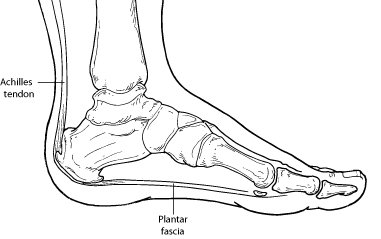
Plantar fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
Causes The most common cause of plantar fasciitis relates to faulty structure of the foot. For example, people who have problems with their arches, either overly flat feet or high-arched feet, are more prone to developing plantar fasciitis.
Wearing non-supportive footwear on hard, flat surfaces puts abnormal strain on the plantar fascia and can also lead to plantar fasciitis. This is particularly evident when one’s job requires long hours on the feet. Obesity may also contribute to plantar fasciitis.
Symptoms The symptoms of plantar fasciitis are:
- Pain on the bottom of the heel
- Pain that is usually worse upon arising
- Pain that increases over a period of months
People with plantar fasciitis often describe the pain as worse when they get up in the morning or after they’ve been sitting for long periods of time. After a few minutes of walking the pain decreases, because walking stretches the fascia. For some people the pain subsides but returns after spending long periods of time on their feet.
Diagnosis To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process the surgeon rules out all the possible causes for your heel pain other than plantar fasciitis.
In addition, diagnostic imaging studies such as x-rays or other imaging modalities may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Non-Surgical Treatment Treatment of plantar fasciitis begins with first-line strategies, which you can begin at home:
- Stretching exercises. Exercises that stretch out the calf muscles help ease pain and assist with recovery.
- Avoid going barefoot. When you walk without shoes, you put undue strain and stress on your plantar fascia.
- Ice. Putting an ice pack on your heel for 20 minutes several times a day helps reduce inflammation. Place a thin towel between the ice and your heel; do not apply ice directly to the skin.
- Limit activities. Cut down on extended physical activities to give your heel a rest.
- Shoe modifications. Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia.
- Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
If you still have pain after several weeks, see your foot and ankle surgeon, who may add one or more of these treatment approaches:
- Padding and strapping. Placing pads in the shoe softens the impact of walking. Strapping helps support the foot and reduce strain on the fascia.
- Orthotic devices. Custom orthotic devices that fit into your shoe help correct the underlying structural abnormalities causing the plantar fasciitis.
- Injection therapy. In some cases, corticosteroid injections are used to help reduce the inflammation and relieve pain.
- Removable walking cast. A removable walking cast may be used to keep your foot immobile for a few weeks to allow it to rest and heal.
- Night splint. Wearing a night splint allows you to maintain an extended stretch of the plantar fascia while sleeping. This may help reduce the morning pain experienced by some patients.
- Physical therapy. Exercises and other physical therapy measures may be used to help provide relief.
When Is Surgery Needed?
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you.
Long-term Care
No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
What is EPAT®?
Extracorporeal Pulse Activation Technology (EPAT®) is the most advanced and highly effective non-invasive treatment method cleared by the FDA. This proprietary technology is based on a unique set of pressure waves that stimulate the metabolism, enhance blood circulation and accelerate the healing process. Damaged tissue gradually regenerates and eventually heals. This non-invasive office/clinic based procedure represents a breakthrough treatment option for a broad range of musculoskeletal conditions.
What disorders can be treated?
Generally, acute or chronic musculoskeletal pain and/or pain that significantly impairs mobility or quality of life.
Areas include:
- Foot and heel pain
- Achilles pain
- Tendon and/or tendon insertion pain
- Neuromas
- Trigger points


What are the possible side effects/complications?
The non-invasive EPAT® treatment has virtually no risks or side effects. In some cases, patients may experience some minor discomfort which may continue for a few days. It is normal to have some residual pain after intense exercise or a full day of work.
Elective Payment and Insurance
Insurance typically does not cover the EPAT® procedure, however, the Elective Payment option allows you to have all the benefits of an EPAT® procedure at a very affordable price. Often there can be significant savings to you through the Elective Payment option as compared to paying deductibles, multiple co-pays, and other non-insurance covered surgery, post operative surgical care and rehabilitation. This non-invasive option will be particularly appealing to those patients who are eager to return to work or normal activities in only a few days with just as good, if not better, clinical results compared to traditional treatment methods, including surgery.
How much does it cost?
For most patients, the Elective Payment out-of-pocket costs are much less than you would expect. Your physician can provide a personalized pricing program. Some patients can use their employer’s “Flexible Payment Medical Savings Account” to cover these out-of-pocket expenses with pre-tax dollars.
How can I get more information?
Your doctor is the best person to talk with if you have questions or concerns about the EPAT® procedure. He or she has extensive knowledge and specialized training on all aspects of its use, safety and effectiveness.
You can also learn more about EPAT® technology by visiting the CuraMedix website at www.curamedix.com.

What are the expected results?
The beneficial effects of Extracorporeal Pulse Activation Technology (EPAT®) are often experienced after only 3 treatments. Some patients report immediate pain relief after the treatment, although it can take up to 4 weeks for pain relief to begin. The procedure eliminates pain and restores full mobility, thus improving your quality of life. Over 80% of patients treated report to be pain free and/or have significant pain reduction.
Is it safe?
Yes. This FDA cleared technology was developed in Europe and is currently used around the globe. A wealth of medical experience, state-of-the-art engineering, and optimal quality have been built into each EPAT® device; and extensive clinical studies and tests have confirmed its safety and efficacy.
If performed by a qualified caregiver, Extracorporeal Pulse Activation Technology (EPAT®) has virtually no risks or side effects.
What is the duration of the treatment and how many treatments will I need?
Treatment sessions take approximately 5-10 minutes depending on the disorder to be treated. Generally, 3 treatment sessions are necessary at weekly intervals.

What will happen after the treatment procedure?
You will receive post-treatment instructions from your physician to follow during your recovery.
What if I have a special health condition?
The safety and effectiveness of the EPAT® procedure has not been determined on people with the following health conditions. Your doctor will provide you with information about how these and other conditions might affect the determination to perform the EPAT® procedures.
- Malignancies
- DVT (Deep Vein Thrombosis)

How is the treatment performed?
Coupling gel is applied to the specified treatment area to enhance effectiveness. After these preparations, EPAT® pressure waves are released via the applicator which is moved over the area in a circular motion.
Why consider non-invasive EPAT®?
EPAT® has a proven success rate that is equal to or greater than that of traditional treatment methods (including surgery) and without the risks, complications and lengthy recovery time. EPAT® is performed in your physician’s office/clinic, does not require anesthesia, requires a minimal amount of time, patients can immediately bear weight (i.e. walk), and return to normal activity within a few days of the procedure.

Benefits of EPAT®
- Non-invasive
- No anesthesia
- No risk of infection
- No scarring
- No downtime
- Over 80% patient satisfaction
- Faster, easier healing
- EPAT Shockwave Brochure
