What is Regenerative Medicine?
- A field of medical, integrative medical, psychological, and social tools to create a sense of healing, youthful responses, and positive outlook.
- Most commonly referred to for medical and cosmetic issues.
Psycho-Social Aspects
- Response to situations
- Response to Illness
- Response to environmental stressors
Turning a response into a reaction to either gain a new perspective or to grow from, and move forward
- EMDR
- Meditation
- Thai Chi
- Other Movement therapies
- Vagal Nerve stimulation/transcranial stimulation
- Many others
Integrative Medicine
- Gut activity and stress response
- Nutritional deficiencies
- Neurotransmitter changes
- Systemic allergies and sensitivities
- Environmental exposures
- Many other fields
- Optimizing the body’s performance
- Using supplementation/herbal/homeopathic
- Energy Medicine
- Acupuncture
- Manual Therapies
- Many more
Medical Thoughts
- To slow the aging process
- To improve the condition of injured and aging tissue
- To improve the function of a person
- To improve the outlook of a person in life
- To avoid risky surgeries and other risks of more invasive treatments
Medial Approaches
- Therapies
- Medications
- Supplements
- Lifestyle modifications
- Injections
- Shock wave Therapy
Therapies
- Electrotherapy
- Manual
- Ultrasound
- Exercises/stretching
Injections
- Hyaluronic Acid
- Helps Joints to maintain spaces and reduce wear and tear
- Helps tissues retain strength, fullness and resilience
- Helps to keep tissues healthier
- Steroids are not generally thought to be Regenerative
- Decreases inflammation for a severe case
- Repeated or large doses cause more aging and tissue thinning; breakdown and more integrity problems
- Trigger Point Injections
- Generally comprised of a numbing medication and various other medications;
- B-12
- Toradol
- Homeopathics
- Other products
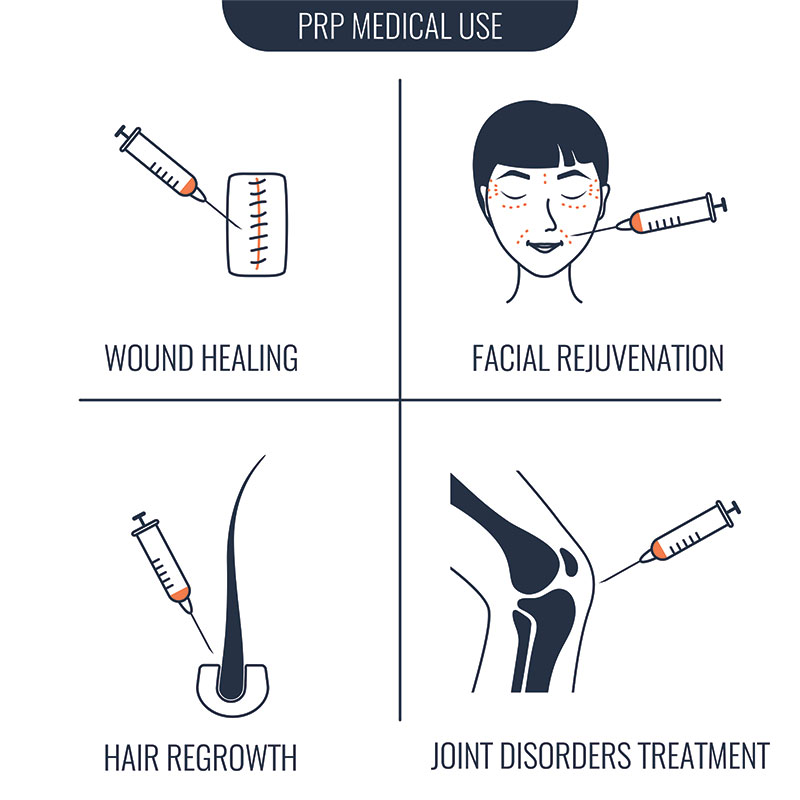
- Platelet Rich Plasma
- Autograft
- Leukocyte Rich
- Leukocyte Poor
- A4M
- Different preparations
- PRP
- Growth factors
- Progenitor cells ; MSC
- Amount decreases with age
- Nutrient rich
- Promotes a healing response
- Bone Marrow or Fat Aspirate
- A true source of functional MSC
- Comes from the patient’s own body or blood matched donor
- Used in many types of surgical and injection therapies
- Extractions can be painful or uncomfortable
Allograft Use
- Typically from a tissue bank that has been ethically and medically inspected an cleared
- Donations by mothers who have delivered a healthy baby of the afterbirth products that had been discarded in years past.
- Umbilical Cord Blood, Uterine lining, placental lining, Wharton’s Jelly
- Contain Growth factors to stimulate a Stem Cell response. Many formulations may not have active live Stem Cell populations.
Exosomes
- Mayo clinic did most initial research
- Many brands now; only counting “cells” but not cell types or sources?
- “Worker Bees” of the stem cell cascade. No actual stem cells in them; not differentiated; so still require a stem cell base in the body to know what to do and where to go.
When it helps
- Arthritic joints
- Tendon/ligaments issues
- Muscle pain
- Spinal issues
- Faster recovery from other modalities; conditions
When Not to do it
- Malignancy
- Infection
- When surgery is absolutely indicated
- Injection precautions
- Performing person is not properly trained
- Facility doesn’t have resources or certification
Cosmetic uses
- Fillers
- Microneedle techniques
- Wound care/scars
- Eyes and other areas
What to know
- Many research projects are actively being done and showing more and more positive uses in many ways
- May not be FDA approved and procedure requires a hold harmless
- New legislation coming in November 2020; many companies have already closed or moved to different products
- Do your homework and always get a second opinion or consider a consultant
- Insurance may cover some of the procedures at this time, so should not be pressured into an expensive cash pay procedure
- Some injections require significant training and should only be done by properly trained physicians
- Some injections require a specific facility or equipment used.
Prolotherapy: Review with background history, mechanism of action, and current evidence
Prolotherapy is a type of therapy that involves injections of an irritant solution into joints, tendons or ligaments to spur an inflammatory response that can expedite healing in damaged tissues.1–3 It is currently used in chronic pain clinics as an alternative treatment for patients who are resistant to the standards of care. It can be utilized in various patient populations, including patients who have knee osteoarthritis, tendinopathy, chronic lower back pain, sacroiliac pain, and other types of chronic pain.4 Prolotherapy shares many similarities to modern regenerative medicine, which focuses on stem cell treatment and tissue engineering to regrow tissue. Prolotherapy can restore joint and tissue function by enabling cells to regenerate and restore normal function without stem cells.5 Patient outcomes have included a reduction in pain/stiffness, improved strength and function, a return to baseline, improved exercise lifestyle, and most importantly, improvement in quality of life.3
Background History Prolotherapy has been used in medicine since 1937.6,7 The physician who developed the therapy, George Hackett MD, initially used it for subluxation of the temporomandibular joint. His conclusion at that time was that sodium psylliate, his proliferant of choice, was a dependable fibrosing agent for long-term stabilization and a return to normal function of the temporomandibular joint. Since then, many proliferants have been used, including glycerine, phenol, platelet-rich plasma, and sodium morrhuate.8 Today, the most used proliferent is hypertonic dextrose. Also known as hyperosmolar dextrose, this injectant is thought to cause remodeling and regeneration of the joint space and to impact specialized cell types like synoviocytes and chondrocytes.9,10
Treatment Schedule Proliferants are usually injected as a series of injections over a specified time period. There are no formal guidelines for prolotherapy, but most institutions have a protocol of solution injection in 2-to-8-week intervals over the course of several months.11–14 Each appointment involves injection of proliferants (thus, the name prolotherapy), and volume varies depending on the type of solution used. Most injections are done in an office setting, and patients may receive topical local anesthetic solutions or subcutaneous lidocaine at the site of injection. Using ultrasound as a guide, articular spaces or tendons and ligaments are identified, and the proliferant is injected. Patients are usually instructed to continue their daily routine or physiotherapy regimen. It is important that patients who are going to receive prolotherapy do not take anti-inflammatory medications because they would prevent the inflammation that is required for cell regeneration.
Mechanism of Action Proliferants such as hyperosmolar dextrose, saline, platelet-rich plasma, mesenchymal stem cells, and hyaluronic acid are injected into intra-articular spaces, enthesis, intervertebral disc spaces, ligaments, and tendons, which leads to irritation and damage to surrounding tissue.3,11,15–17 This induces an immune response at the site of injection, resulting in hypertrophy and hyperplasia of damaged tissue.13 This inflammatory response creates stronger tissue and matrix structure, which in turn improves joint stability, function, and tendon/ligament attachment.13 Platelet-rich plasma is generally evaluated to be a safe and effective means of prolotherapy.11,16,18 Platelets have innate immune modulatory properties. When activated, cytokines and growth factors are released that play a role in cell growth, cell recruitment, and cell repair.19–22 This proves to be advantageous for cells that do not have innate healing abilities such as cartilage. A study by Cole et al found a statistically significant decrease in IL-1ß and TNF-α within the knee when platelet-rich plasma was used as the proliferant agent versus hyaluronic acid, suggesting that there are anti-inflammatory properties contributing to improvement of osteoarthritic symptoms.23 The combined effects of prolotherapy are hypothesized to result in decreased pain that enables patients to reach their original baseline.13,16
Hyperosmolar Dextrose Hyperosmolar dextrose is the most popular type of prolotherapy because of its safety profile, cost effectiveness, and water-soluble properties.24 Hyperosmolar dextrose (10-30%) causes osmotic shock to synoviocytes, which acts to dehydrate the cells.4 This cellular damage causes a release of cytokines and growth factors that lead to migration of macrophages and neutrophils, and eventually to cellular and tissue proliferation.25–27 The result is new cells, tissue, and matrix deposited at the damaged site. Dextrose prolotherapy has been used for chronic musculoskeletal pain, lower back pain, sacroiliac joint pain, and knee and ankle osteoarthritis.28 A meta-analysis by Nagori et al looked at the efficacy of dextrose prolotherapy over placebo for temporomandibular joint hypermobility and found a statistically significant reduction in pain and maximal mouth opening versus placebo.28 The metanalysis was limited by the total number of studies included. A 2020 randomized control trial by Chung et al looked at intraarticular dextrose prolotherapy vs hyaluronic acid and found a statistically significant difference in immediate pain relief up to 3 months for patients who received hyperosmolar dextrose vs those who received hyaluronic acid.12
Conclusions Overall, prolotherapy is a safe in-office procedure. A recent meta-analysis by Bae et al. found that hyperosmolar dextrose prolotherapy provided pain relief similar to that provided by platelet-rich plasma or steroid injection. The meta-analysis also found that hyperosmolar dextrose prolotherapy was more effective in the treatment of chronic pain than saline injection or exercise.5 A majority of the literature focuses on knee osteoarthritis, while literature discussing the use of prolotherapy for other articulating joints is lacking. There is mounting evidence that prolotherapy should be used in clinical practice, and that it is becoming a commonly employed therapy in chronic joint patients. To establish the true benefit of prolotherapy, more randomized control trials with longer durations, larger sample sizes, and standardized protocols are required. Such trials would allow the chronic pain community to establish guidelines and more uniformity as to which proliferant would produce the best outcomes for chronic joint-pain patients. Prolotherapy continues to be an important topic of discussion in the field of chronic pain. Further research to determine optimal proliferants and the number and timing of injections would be beneficial for the clinical utility of this therapy.





















