Finding and Blocking a Trigger Zone using a Q-tip Test
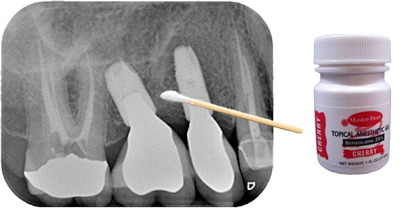
When a patient is complaining about pain and the teeth have been ruled out as a cause, the dentist should see if he/she can find the trigger zone and replicate the pain using a Q-tip. First, ask the patient to describe where the pain is occurring and, even better, give them a Q-tip to show you where they are feeling pain. Then using a very light touch with the Q-tip, try stroking the tissue around the area where the patient is reporting their pain and ask them if that hurts. Then try pressing on the same area with firm pressure and ask them if that hurts. If you are able to replicate the pain using either of these techniques then the next step is to see if you can reduce or block the pain. Apply a topical anesthetic to the area where you caused the pain with a Q-tip. Wait a few minutes and repeat the Q-tip test to see if you can replicate the pain. Next, try infiltrating the papilla or local tissue where you were able to replicate the pain and repeat the Q-tip test. Last, try blocking the tooth as if you were going to do a restoration and repeat the Q-tip test. If you have ruled out an odontogenic cause of the pain, and any of these methods greatly reduce or block the pain, then it is likely a neuropathic pain of the trigeminal nerve. If you cannot block any of the pain, then the pain is centralized. The next step, especially in the case of pain on the maxillary arch, is to try is a sphenopalatine ganglion block (SPG). This can be done in the office. I use a Sphenocath with 2 cc's of 4% lidocaine into the nostril on the ipsilateral side of the pain. If you can block the pain using an SPG block, repeat the procedure once a week for a total of six weeks. This will hopefully provide the patient with pain relief for six months or longer.
An important piece of this pain puzzle to keep in mind is if the pain started on its own or if the pain started after a dental procedure or any trauma. If it started on its own, is intermittent, and is described as a sharp, shooting electrical pain then it is likely trigeminal neuralgia, which can be treated with anti-seizure medications and an MRI must be ordered. If the pain started after a dental procedure, you have ruled out the tooth, is described as a burning pain that does not go away, and you can reduce the pain or completely block it, then it is likely a painful post-traumatic trigeminal neuropathy (PPTN), which can be treated topically.
Technical Terms
Allodynia - a painful response to a non-painful stimulus. A great example is skin that has a sunburn, which is painful to the touch. Skin does not normally hurt.
Ephaptic transmission - when light touch triggers pain, the A-beta fibers have undergone a transformation from sending a non-painful signal to a painful signal.
Dynamic mechanical allodynia - pain with light touch.
Static mechanical allodynia - pain with firm pressure.
A-beta fibers - responsible for the sensation of touch. The fibers are myelinated.
A-delta fibers - responsible for the sensation of pain from mechanical and thermal inputs. The fibers are myelinated. These are the "fast pain" fibers such as what you feel when you stick your finger over a fire.
C fibers - responsible for the sensation of pain from mechanical, thermal, and chemical inputs. The fibers are unmyelinated. These are the " slow pain" fibers, which are what cause pain that lingers.